Accidentally sending medical information to the wrong person is a serious data privacy breach that can expose sensitive health information (PHI) and violate privacy laws such as HIPAA.
Whether you’re a healthcare provider, business associate, or even a patient who inadvertently shares personal health details, it’s essential to know the steps to take to minimize harm, comply with legal obligations, and rebuild trust.
Why Medical Information Disclosure Matters
Medical records often contain highly sensitive data, including diagnoses and treatments, billing information, and personal identifiers. When this information is sent to the wrong person, it could:
- Compromise patient privacy
- Result in identity theft or fraud
- Damage your organization’s reputation
- Lead to regulatory penalties or lawsuits
Healthcare organizations have a legal and ethical responsibility to handle such incidents swiftly and responsibly.
Common Scenarios of Misdelivery
Medical information can be sent to the wrong person through various means, including:
- Email or Fax: A mistyped email address or fax number can result in unintended disclosure.
- Postal Mail: Incorrect mailing labels or address errors can result in records being sent to the wrong recipient.
- Verbal Communication: Discussing PHI in a non-secure environment can lead to unintended eavesdropping.
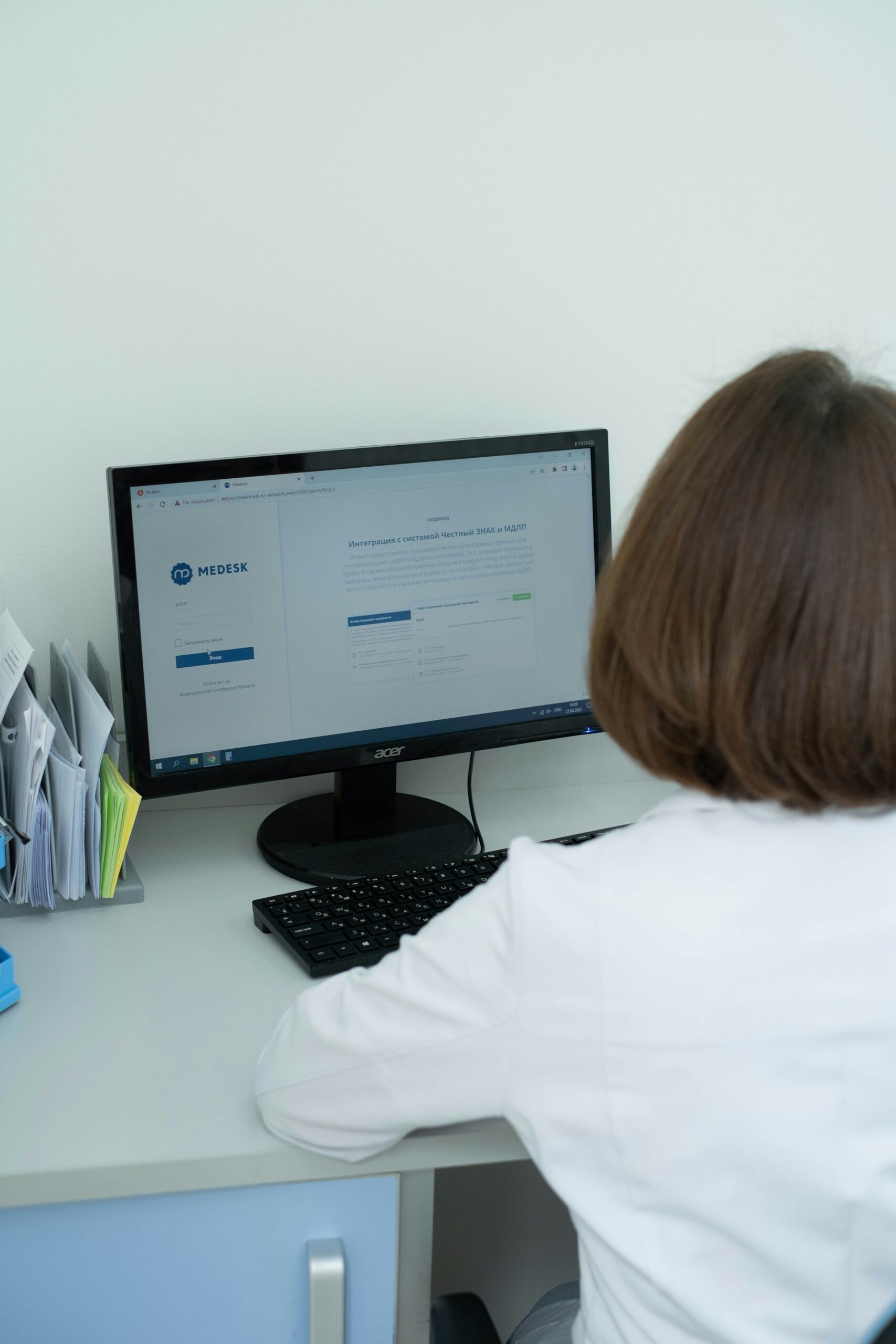
- Electronic Health Records (EHR) Portals: Incorrectly assigned user credentials may allow unauthorized access.
Immediate Steps to Take
Here are the steps to follow if a medical record is sent to the wrong individual by accident.
1. Verify the Disclosure
Start by confirming that PHI was indeed sent to the wrong recipient. Check:
- The type of information disclosed (e.g., test results, billing records)
- The method of disclosure (email, fax, mail)
- Whether the recipient received or accessed the information
2. Notify Your Privacy Officer or Compliance Department
If you’re part of a healthcare organization, immediately notify your Privacy Officer or Compliance team. They are responsible for coordinating the breach response process and ensuring compliance with regulations like HIPAA.
3. Retrieve or Secure the Disclosed Information
If feasible, contact the recipient and request the return, secure destruction, or deletion of the information. Provide clear instructions on how to handle the data to prevent further exposure.
4. Document the Incident Thoroughly
Create a detailed record that includes:
- The date and time of the breach
- The recipient’s information
- The type and amount of data disclosed
- Steps taken to mitigate harm
- Any communications with the recipient
This documentation is critical for internal reviews and, if necessary, for reporting the incident to regulatory authorities.
5. Perform a Risk Assessment
Evaluate the potential impact of the breach by considering the following:
- The sensitivity of the disclosed information (e.g., mental health records vs. billing info)
- The relationship between the recipient and the patient
- The likelihood of the recipient further disclosing the information
- The probability of identity theft or financial harm
This assessment helps determine whether the breach needs to be formally reported under the Health Insurance Portability and Accountability Act (HIPAA).
6. Notify the Affected Individual(s)
Under HIPAA, patients must be notified “without unreasonable delay” and no later than 60 days after the discovery of the breach. The notice should include:
- A description of the breach
- What information was involved
- Steps you are taking to investigate and mitigate the breach
- Contact information for questions or assistance
Timely and transparent communication helps maintain patient trust and confidence.
7. Consider Regulatory Reporting
If the risk assessment indicates a high probability of compromise, report the breach to the U.S. Department of Health and Human Services (HHS) Office for Civil Rights (OCR). Some state laws may also require notification to state authorities or consumer protection agencies.
8. Review Policies and Retrain Staff
After the incident, review your organization’s privacy and security policies to identify gaps or weaknesses. Provide additional staff training to reinforce best practices in handling Protected Health Information (PHI).
Legal and Regulatory Considerations
HIPAA defines a “breach” as any unauthorized acquisition, access, use, or disclosure of protected health information (PHI) that compromises its integrity, security, or confidentiality. Not every incident qualifies as a reportable breach. If the organization can demonstrate a low probability of compromise (based on factors such as data type, recipient, and mitigation efforts), the incident may not require formal reporting. However, documentation of this risk assessment is still needed.
State laws may vary in their definitions and requirements for breach notification. Always consult your compliance team or legal counsel to ensure adherence to both federal and state regulations.
Preventing Future Incidents
Prevention is key to protecting patient privacy and avoiding costly penalties. Here are some best practices:
- Double-Check Recipient Details: Always confirm email addresses, fax numbers, and mailing addresses before sending PHI.
- Use Secure Communication Channels: Implement encryption for emails and secure fax lines for transmitting PHI.
- Access Controls: Restrict EHR and file system access to authorized staff only.
- Regular Training: Educate staff on privacy practices, standard errors, and reporting protocols to ensure compliance.
- Audit Trails: Monitor access logs to detect unauthorized access early.
Conclusion
Mistakenly sending medical information to the wrong person can have serious consequences, but by acting quickly, documenting the incident, notifying the proper parties, and strengthening your privacy practices, you can mitigate the impact and prevent future breaches.
Staying proactive helps you maintain patient trust, comply with legal requirements, and safeguard sensitive health information.
What qualifies as a breach under HIPAA?
A breach is any unauthorized acquisition, access, use, or disclosure of PHI that compromises its privacy or security.
Should I notify the patient if their information was sent to the wrong person?
Yes, HIPAA requires notification of the affected individual(s) without unreasonable delay and within 60 days of discovery.
What if the recipient is a family member or friend of the patient?
Even if the recipient knows the patient, it’s still considered a breach. A risk assessment will determine if the breach is reportable.
Can I be fined if I accidentally send medical information to the wrong person?
Yes, healthcare providers can face significant fines for HIPAA violations. Penalties depend on the nature and severity of the breach, as well as the organization’s compliance history.